Cleanroom News, Cleanrooms, FDA
Is Bigger Necessarily Better?
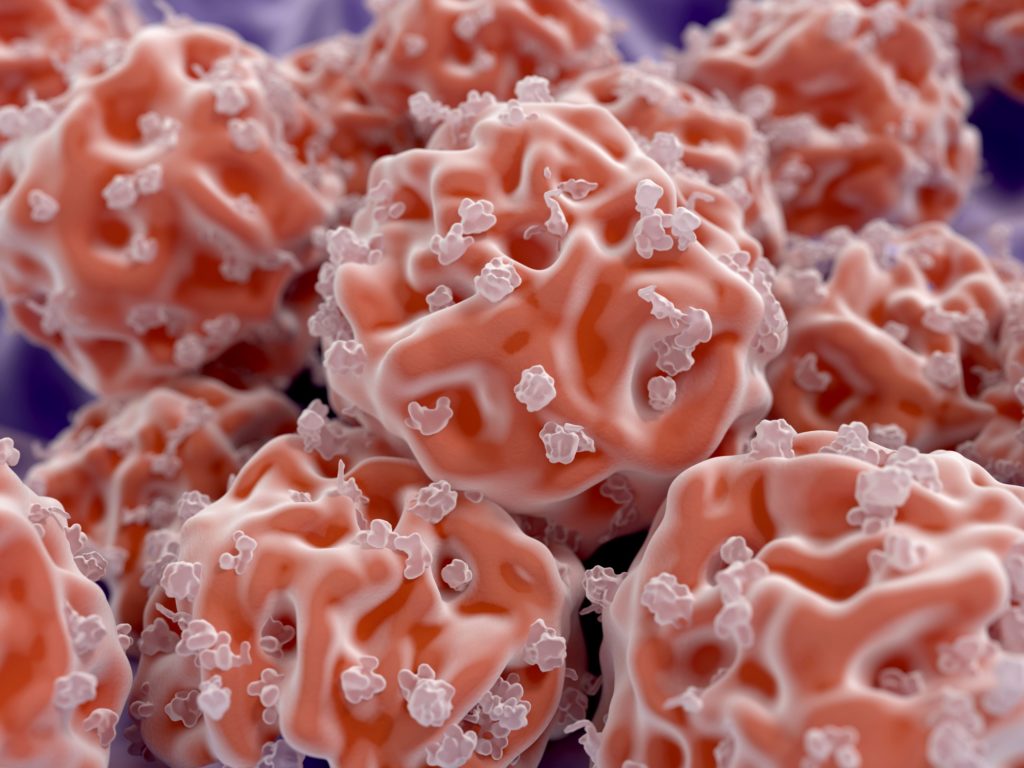
No-one wants to imagine the unimaginable. You feel vaguely unwell but can’t quite put your finger on the cause. Your significant other pushes you to make that doctor’s appointment – ‘just to put your mind at ease.’ Your family doctor runs a few tests and, ‘without wanting to alarm you unduly,’ refers you up the chain to a specialist. A week goes by until your appointment. Now you’re sitting nervously in the specialist’s office at the oncology center. She’s explaining things and mentally you’re running as fast as you can to keep up with her. She’s speaking a whole new language, one that defines the terrain of your inexplicably shifted landscape. Haematopoiesis. Stem cells. HSCs. Gene expression. You listen, but at this point not much of it makes sense.
From a patient’s perspective, this is the challenging reality of a clinical diagnosis of cancer.
From a clinician’s perspective, the territory is well known and the challenges lie not in its navigation but in readying the equipment for the journey. And this is where a new development in the field of blood-separation technology has turned conventional protocol on its head. Until now, stem cell manipulation required the use of a highly specialized cleanroom staffed by expertly trained personnel. At St Jude’s Children’s Research Hospital in Memphis, TN, for instance, a 60,000 square foot facility is used to separate the stem cells from a patient’s blood or bone marrow so that they can be reintroduced to the patient after genetic correction. Dr. Brian Sorrentino likens the process to “being a surgeon in an operating room, except that here we’re operating on cells.”(1)
And the analogy is apparent. For gene therapy researcher Jennifer Adair of Fred Hutchinson’s Cancer Research Center in Seattle, WA, the process of working within an OR-like cleanroom environment was onerous. During an experimental study on a patient with brain cancer, every time she stepped out of the sterile environment, she was forced to follow contamination control procedures upon re-entry including scrubbing, cleansing, and gowning. While knowing that humans are the biggest source of cross contamination in a cleanroom environment she still felt this represented a waste of time and effort and that a better way had to be possible. Seeing the need to streamline the process and to expand its reach to the broader range of patients in need, Adair created a benchtop machine that she calls ‘gene therapy in a box.’
“Gene therapy in a box”
In essence, the box is a portable cleanroom in miniature. Collaborating with German medical technology partner Miltenyi Biotec, Adair created a closed-system cell processor, the Prodigy machine, that isolates stem cells in a sample of blood or bone marrow, separating them into an IV bag for reintroduction into a patient following gene therapy. The ability to genetically modify stem cells – also known as hematopoietic stem cells or HSCs – is critical to treating disorders such as sickle cell anemia or beta-thalassemia, a disorder in which the production of hemoglobin is severely compromised. The initial reception of Adair’s lab in a box has been encouraging, with Rocket Pharmaceuticals of New York, a player in the gene-modified cell therapies market, investing heavily in funding it to market. According to a company source, Rocket Pharmaceuticals hopes to fund a trial for patients with Fanconi anemia – a severe condition that affects bone marrow and increases the risk of some cancers – as soon as 2017, having seen the Food and Drug Administration’s early approval of the Prodigy machine.
So what exactly is it about Adair’s system that has heads turning in both the industry and the FDA? Part of the appeal is very simple: portability. Let’s back up… We’ve talked before about the innovation of miniaturization – check out Honey, I Shrunk the Lab, for instance – and creating the technology necessary to replicate large systems in more mobile, accessible, user-friendly, and efficient ways is becoming something of an industry Holy Grail. And perhaps this is especially true in the biomedical field. Whether treating contagious outbreaks like ebola in the field or bringing modern technology to geographically isolated communities, miniaturizing large-scale equipment is a crucial 21st century weapon in the war against disease. By porting the power of a high-tech cleanroom to an impoverished community in the grip of HIV, for instance, medics can offer treatment (and hope for a future) to individuals where they are – at the point of care. Adair and other researchers believe that the portability of specialist equipment holds enormous potential for saving lives, eliminating one of the two main barriers to treatment. The second one – cost – is also something she’s working on.

In the case gene therapy, for example, we know that although it’s effective in treating a range of conditions, from cancers to HIV, the price tag can be prohibitive. And one part of the expense is the necessary use of a sterile environment, both for modifying blood cells and for manipulating their genetic structure. In other words, although absolutely critical, the need for a cleanroom is a limiting factor in terms not only in terms of availability but also of cost. In her early work, Adair noted that patients are not often located proximal to a top-tier institution that might have access to a cleanroom but, with a portable lab, availability goes up and costs come down significantly. For instance, according to Genetic Engineering & Biotechnology News, the cost of a ‘gene therapy in a box’ would start at approximately $150,000 as a one-time investment that could offer treatment to many thousands of patients.(2) And that is a cost that many hospitals, clinics, or field stations could conceivably bear. Furthermore, with the widespread adoption of the Prodigy or its successors, the cost per unit would scale down, making it even more accessible to later adopters.
But what about safety? How can clinicians and patients be certain that the process is as safe as it can possibly be? At this stage of development, Adair’s unit can be used to pull stem cells from a blood sample, add nutrients to facilitate their growth, and add a viral vector to enable a gene transfer, depending upon the specific disease being treated. The modified cells are subsequently transferred back to the patient via a sterile bag connected to an IV. And even with such a comparatively simple operation, it’s easy to see how critical absolute sterility is to the success of the treatment. During the traditional pharmaceutical manufacturing process, a media fill would be used to ensure sterility of the equipment – can we assume that this will also be the case with the lab in a box?
Another planned future use of Adair’s device is for in-vivo gene therapy, wherein the ‘intravenous administration of non-pathogenic viral vectors allows cells to receive corrective genes within their native environments.’(3) In other words the blood remains within the patient during treatment. Although tested so far only on non-human subjects, the technique looks promising, especially given that its associated reduction in cost would make the therapy more widely available. But again, the issue of safety weighs heavily on our minds. Can we trust this ‘black box’ to be utterly sterilized – and sterilizable – between patients?
One thing we know for sure at this stage is that either of these processes – and indeed any operation that includes the isolation of cells within a portable closed-system – must conform to the same Current Good Manufacturing Practice (cGMP) as those in place within a regular contamination-controlled facility. CGMPs are designed to ensure the correct monitoring and control of processes and facilities, and to regulate strength, quality and purity of the final product. They govern quality assurance tasks, in other words. When correctly devised, implemented, and followed cGMPs are able to prevent or detect errors, contamination, deviations or failures, ensuring the safety of consumers – in this case, patients – down the line. And perhaps the most important component of these guidelines is their inherent flexibility: the ‘c’ standing for ‘current,’ underlining the fact that they must be flexible and adaptive. They must stay up to date, strive for continual improvement, and be in compliance with existing and future regulation.
And the Prodigy machine complies with all of that. According to Adair, the FDA has already approved her innovation and, given that Naveen Yalamanchi, Roderick Wong, and Gaurav Shah of Rocket Pharmaceuticals have raised almost $16.5 million in a securities offering filed with the SEC, the future is looking promising.(4) And, with the right backing, it’s one that is almost infinitely adaptable and could be tailored to any specific disease. As Adair remarked in her GE&BN interview, “by making a platform that doesn’t require you to be at one of the expert academic institutions for gene therapy, we’re facilitating more people being able to explore these processes and potentially incorporate their own changes.”(5) And as long as the ‘c’ in cGMP is respected, an exciting adventure in gene science awaits.
Do you have thoughts on miniaturization and automation as they apply to the biomedical field? We’d love to hear them! Please share your ideas in the comments section below!
References:
- http://www.xconomy.com/seattle/2016/10/20/fred-hutch-team-wants-to-move-clean-room-gene-therapy-to-tabletop/?single_page=true#
- http://www.genengnews.com/gen-news-highlights/point-of-care-gene-therapy-is-out-of-the-box/81253344
- http://research.fhcrc.org/adair/en/collaborations/portability.html
- https://www.sec.gov/Archives/edgar/data/1663128/000166312816000002/xslFormDX01/primary_doc.xml
- http://www.genengnews.com/gen-news-highlights/point-of-care-gene-therapy-is-out-of-the-box/81253344
Additional references:
http://www.miltenyibiotec.com/en.aspx
http://research.fhcrc.org/adair/en/collaborations/portability.html
http://www.rocketpharma.com




















Pingback: Caja de Gene thearapy portátil es este el futuro de la sala blanca? - Productos Para Cuartos Limpios|Berkshire Mexico
Pingback: Is Bigger Necessarily Better? - Berkshire Singapore
Pingback: Is Bigger Necessarily Better? - Cleanroom News ...