Cleanroom News, Cleanrooms
Cancer, Cocoons, and the Cleanroom.
If it’s been a long week already perhaps you’re in the mood for a little light relief for your Thursday. So here’s a quick quiz to see whether you – our readers – pay as much attention to broader culture as you do to news from within our industry. So without further ado, here’s our pop-quiz question: Which movie featuring ‘Antareans’ was a surprise Box Office hit in 1985?
No Googling! (We’ll know if you did!)
OK, time’s up. If you said ‘Cocoon,’ a film directed by Ron Howard which grossed over $76 million dollars, you’d be right.* The conceit of this (loosely sci-fi) movie was the thwarting by a huddle of Florida retirees of a group rescue of extraterrestrials, cocooned for millennia on the ocean floor. Having stumbled upon plan, the seniors subsequently become aware that their new neighbors also possess the secret of eternal youth. Availing themselves freely of the rejuvenating waters of the backyard swimming pool – in which the rescued cocoons are temporarily stored – the seniors begin to wind back the clock of advancing age and physical disease and decline, ultimately achieving eternal life through the technology of the extraterrestrial visitors.
It was a sweet, sometimes cheesy, and now definitely dated treatment of the fountain of youth mythos, a feel-good film that invited gentle reflection on the theme of aging. And such light relief was certainly needed in a year when, across the Pond, the British Film and Television Awards (BAFTAs) recognized the searing portrayal of the Cambodian civil war in ‘The Killing Fields’ in its Best Film category, and French film-maker Claude Lanzmann debuted his ground-breaking holocaust documentary, ‘Shoah.’
Yes, this was a fun trip down Hollywood’s ‘memory lane,’ but what does it have to do with our topic of the day, cancer, cocoons, and the cleanroom? We’re glad you asked! More than three decades after the release of ‘Cocoon’ technology is now being developed that has the potential to bring us one step closer to the dream of physical longevity in which disease is eradicated. And when it comes to one of the most feared diseases, an innovation known as the ‘Cocoon’ is playing an integral role in bringing this vision to fruition.
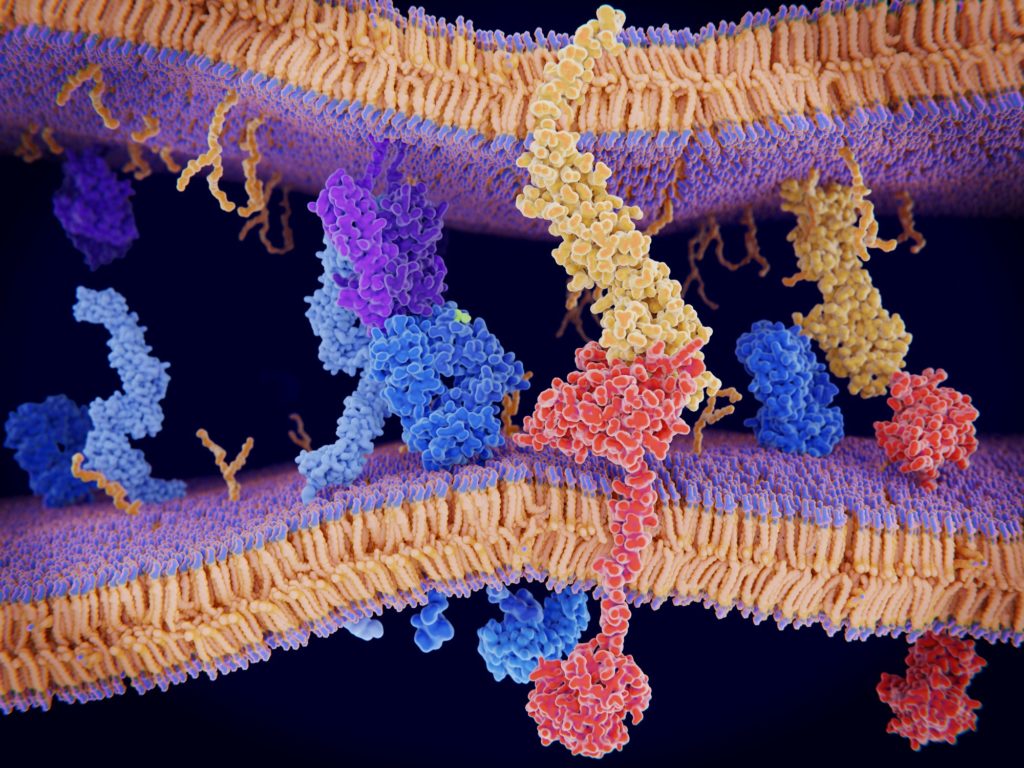
Cancer. It’s a diagnosis that is almost guaranteed to provoke considerable anxiety. Desperate images of physical wasting, pain, helplessness, and ultimate loss swirl around those two syllables which have, in the past, seemed like a death sentence. But times are changing. According to the American Society for Clinical Oncology, statistics show that we have significantly less to fear from the disease today than at any other point in medical history. In an article entitled ‘Advances in Cancer Treatment,’ the society notes that ‘Treatment advances across the spectrum of cancers have continued at a rapid pace […] primarily in immunotherapy [but also in] systemic chemotherapy, targeted chemotherapy, surgery, and radiotherapy.’(1) In other words, alongside additional improvements in treating solid tumor and blood cancers, immunotherapy is being shown to increase survival gains in patients treated with a combination of approaches. So significant is the advance in our understanding of this type of therapeutic approach, in fact, that two researchers working independently on harnessing the immune system were awarded the Nobel Prize for medicine last year. James P. Allison of the University of Texas and Tasuku Honjo of Kyoto University pioneered work on manipulating proteins that act as a braking mechanism in the immune system’s fight against cancerous cells. By disabling this protein, PD-1, in mice Honjo found that their immune systems ‘went into overdrive’ and the mice did not go on to develop tumors. From this discovery, PD-1 inhibitors such as nivolumab and pembrolizumab were created, drugs which have seen exciting results on shrinking tumors more efficiently than conventional chemo- or radiotherapy. And here in the U.S., Allison discovered that using an antibody to block another protein, CTLA-4, allowed patients’ immune systems to work more efficiently and rapidly in locating and destroying cancer cells. Allison’s work resulted in the creation of the drug ipilimumab which, in 2011, was the first ‘checkpoint inhibitor’ to be approved by the U.S. Food and Drug Administration (FDA).(2) But what is a checkpoint inhibitor and why is it significant in terms of T-cells and the immune system?
This is where the research starts to get very interesting. The function of the body’s T-cells is to hunt down and destroy cells that could cause physical infection. Think of them as an elite SWAT team with only one mission: seek and destroy invaders wherever they hide. However when it comes to cancer, both the T-cell SWAT teams and their back-up operatives – the Helper T-cells – have traditionally offered a less than elite response. And this sub-standard performance is due to the presence of certain proteins such as PD-L1 which are produced by the tumor cells to bind to the T-cell’s PD-1 protein. In effect, this binding of PD-1 and PD-L1 results in a hobbling of the immune system such that the T-cells are unable to accomplish their mission. However, by introducing a checkpoint inhibitor such as those developed by Allison and Honjo, receptors are effectively ‘gummed up’ or blocked, strengthening the T-cell sufficiently to cause cell death in the tumor. Mission accomplished.
So with an increase in T-cell efficiency, a cancer patient stands a greater chance of halting the progression of the disease and perhaps even eradicating it. But what if we could increase not only the efficiency of the body’s T-cells but also their number? What if we could recruit more elite SWAT team members, swell their ranks, and provide a veritable army of protector cells to swarm tumorous cells and neutralize them?
This, of course, is where advances pioneered by the Sheba Medical Center in Tel Hashomer, Israel, in partnership with Swiss pharma giant Lonza Group, are so exciting.
Developed at the Weizmann Institute of Science, a radical new form of immunotherapy involves the custom modification of a patient’s own T-cells on a molecular level. The genetically modified T-cells, known as Chimeric Antigen Receptors (CAR) T-cells are better able to hunt down and eliminate cancer cells on an individual basis forming what Professor Dror Harats, deputy director for research and development and director for clinical trials at the center, described as ‘a new era of cell therapy.’(3) Indeed, he continued, this is ‘a precision medicine, where we take the cells from the patient, molecular-engineer them, and then give it back to the patient.’(4)
So where does that leave facilities without the budget for state-of-the-art cleanroom environments?
But in order to genetically modify human cells to create this rapid reaction force of CAR-T SWAT teams, any research or medical facility needs access to a top-of-the-line cleanroom. And as we know the cost of constructing and maintaining this sort of facility can be prohibitive. Be that as it may, as Harats noted in interview with The Times Israel, ‘“When you do cell therapy like this you need to work in a completely clean environment, with clean rooms — and that always limits the number of patients that you can actually treat.”’ So where does that leave facilities without the budget for state-of-the-art cleanroom environments? Let’s take a moment to circle back to the Cocoon…
Developed as a podular (think modular, but with pods) system, the Cocoon is based on a GMP-in-a-box concept platform and is comprised of banks of hanging pods each of which contains a small bioreactor. (For more on bioreactors, see our earlier article, ‘How Bioreactors and Cleanroom Technology Might Be the Answer To Declining Seafood Stocks.’)The automated pods function as incubators, growing CAR-T cells on an on-demand basis for multiple individual patients. And, according to Lonza, the up-scaling of solutions does not come with any increase in contamination risk. Each Cocoon is a ‘closed, automated, highly flexible cell therapy manufacturing platform’ that offers ‘end to end manufacturing […with] key unit operations, including isolation, activation, traduction, expansion, and harvest.’(5) The manufacturing process is fully enclosed, employing single-use cassettes with minimal touchpoints in the process. Variables such as temperature, humidity, pH levels and gases are also monitored, with batch records generated for full documentation and product traceability. Moreover, where the Sheba Medical Center could treat perhaps four patients per month using a traditional cleanroom, says Harats, the Cocoon will allow the engineering of hundreds of batches of cells, offering hope to a correspondingly increased number of individuals and bypassing the conventional bottleneck of cell therapy manufacturing. Trials of patient-scaled CAR-T immunotherapies have already shown promise in individuals whose condition has been resistant to more conventional therapies, and trials on leukemia and lymphoma patients are expected to commence shortly.
A casual glance at some of the product images of the Cocoon reveals a sleek, futuristic bank of capsules that certainly give the impression of space age technology harnessed in the service of an age old disease. This X-factor lends a confidence to the company’s description of on-going trials with ‘select partners’ that Lonza, a solutions provider that serves the healthcare, biotech, and nutrition markets, hopes will demonstrate ways in which the Cocoon will address needs from pre-clinical to commercial-scale manufacturing in the cell therapy arena. We will certainly be watching this technology continue to develop and hope to bring an update in due course.
With that said, there is another potential solution available for medical or research institutions without the necessary budget for fully-fledged, dedicated cleanroom facilities: the POD. Although the term is readily familiar as a relatively simple method of household relocation or to coffee drinkers in need of a quick brew, PODs in this context refer to prefabricated and often autonomous facilities offering cleanroom equipment and technologies at a fraction of the cost. Engineered by G-CON Manufacturing Inc., a Texas-based company that focuses on the pharma and biopharma markets, the PODs are scalable units, designed for specific purposes such as aseptic fill/finish, product processing platforms, or research and development environments, and can be repurposed from one specific use to another. This is an innovation we’ll be examining in greater depth next time, so stay tuned…
Certainly, the Cocoon and the POD platforms are exciting developments in the field and will potentially facilitate significant strides forward in developing innovative, targeted, and customized treatments for cancer in all its variations.
Of course, it goes almost without saying that regulation of these technologies is still a somewhat uncertain landscape. As we noted last year in our article ‘How the Promise of Stem Cell Therapy Can Blind Us to Its Danger’, stem cell therapy, used to combat myriad disorders including cancer, is still in its infancy and only certain therapeutic protocols are sanctioned by the FDA. And in the field of immunotherapy, this is equally true. However, there are two parts to this issue – the therapies themselves and the equipment used to facilitate them.
Certainly, the Cocoon and the POD platforms are exciting developments in the field and will potentially facilitate significant strides forward in developing innovative, targeted, and customized treatments for cancer in all its variations.
And in this respect, we are thrilled to witness how a combination of intellectual curiosity and scientific expertise is pushing on the frontiers of technology and making new therapies available to ever-increasing populations so desperately in need of them.
What do you think? Is the future of oncology in the design of genetically modified T-cells, customized to each patient as needed? Do you think there is a better way and that this new tech is just a stepping stone along the path to the eradication of cancer? We’d love to know your thoughts.
References:
- https://www.asco.org/research-progress/reports-studies/clinical-cancer-advances-2019/advances-cancer-treatment
- https://interestingengineering.com/2018-medicine-nobel-prize-awarded-to-two-cancer-immunologists
- https://www.timesofisrael.com/replacing-clean-rooms-sheba-hospital-to-use-pods-to-grow-cancer-killing-cells/
- ibid
- https://www.lonza.com/products-services/pharma-biotech/bioprocess-systems/patient-scale-cell-manufacturing.aspx
*Extra credit goes to those who can name the actor who starred in both Cocoon and in the highest grossing movie of 1989…


















HAVE AN IDEA FOR CONTENT?
We are always looking for ideas and topics to write about.
Contact Us